Introduction
Primary ciliary dyskinesia or PCD is an inherited disease characterized by infertility, the inability to have children, persistent respiratory tract infections, and improperly positioned internal organs. The symptoms and signs of this illness are brought on by aberrant flagella and cilia.
What Is Primary Ciliary Dyskinesia?
Primary ciliary dyskinesia, or PCD, is an infrequent inherited disease (“Inherited disorders” are the disorders passed from parents to children, mediated by genes), that affects the tiny, hair-like structures (cilia) lining mainly the airways.
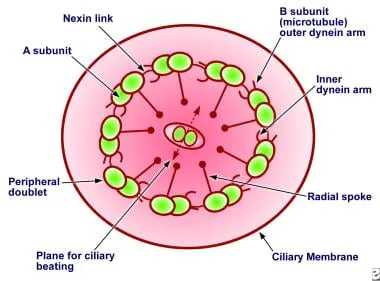
- Ciliaare tiny, finger-like hairy projections that pop out from the cell’s outside. Their occurrence sites include the linings of several organs and tissues, including the respiratory airway and reproductive systems. These cilia help in carrying mucus (a slimy substance) toward the mouth to be coughed or sneezed outside the body. The mucus contains inhaled impurities, along with air, dust, bacteria, and other small particles.
- Flagella are cilia-like structures with a tail that aid sperm cells to move forward.
Consequences or Symptoms of Primary Ciliary Dyskinesia
- Some people are born with problems with the cilia that prevent them from moving the mucus out of the airways. This causes mucus to build up and leads to infections and problems related to breathing. PCD affects the sinuses, lungs, and ears.
- Some PCD patients have congenital(from the moment of birth) breathing problems, which marks the importance of cilia in removing amniotic (or fetal) fluid from the lungs.
- Affected people frequently get respiratory tract infections starting at a young age. Because the cilia in the airway aren’t working properly, bacteria can stay in the respiratory tract and lead to life-threatening illnesses.
- Continuous nasal congestion and a persistent cough are additional symptoms of primary ciliary dyskinesia. Persistent respiratory tract infections produce bronchiectasis, a unique disorder that affects the bronchi, and the airways that connect the trachea to the lungs and results in potentially fatal breathing difficulties.
- Defects related to organs: Organ placement in thoracic and abdominal cavities can be incorrect in certain people with primary ciliary dyskinesia. These anomalies appear during the development of the embryo.
- Situs inversus totalis: The internal organs of about 50% of PCD patients are reversed in mirror images. The whole situs inversus has no discernible negative effects on health. If a person has both situs inversus totalis and primary ciliary dyskinesia, the condition is known as Kartagener Syndrome.
- Situs ambiguous: Situs ambiguus or heterotaxy syndrome, which is defined by abnormalities of the heart, liver, intestines, or spleen, affects about 12% of persons with primary ciliary dyskinesia. The term “situs ambiguous” refers to an anomalous placement of thoracoabdominal organs. This is due to issues with how the left and right sides of the body are shown during embryonic development.
- Infertility:Since the sperm cells must be propelled forward to the female egg cell by powerful flagella motions, infertility occurs in individuals suffering from PCD due to the immobility of cilia. Infertility in affected males is caused because their sperm do not migrate properly, whereas, in the case of affected females, they have infertility as a result of damaged fallopian tube cilia.
- Otitis media: PCD also causes repeated ear infections known as Otitis Media, mainly in children. These infections are likely due to the inner ear cilia that aren’t normal. If left untreated, it might lead to permanent hearing loss.
Causes of Primary Ciliary Dyskinesia
- As an inherited condition, primary ciliary dyskinesia (PCD), commonly referred to as immotile cilia syndrome, is mediated by genes. Yet, this procedure gets incredibly difficult when PCD is included. The disease’s inheritance pattern and the genes involved are still being investigated by researchers.
- As a recessive disorder, PCD can only be acquired through the inheritance of defective genes from both parents. These genes may impact cilia’s ability to develop, function, or both.
- The cilia may have the incorrect size, shape, or movement due to faulty genes. Sometimes the cilia may even be completely absent. Ineffective cilia allow bacteria to remain in your airways. This causes breathing problems and other infections.
- In case a defective gene (or genes) is inherited by a child from only one parent, the child then is only a “PCD carrier.” Often, carriers do not exhibit PCD symptoms. But, carriers can transfer defective PCD genes to their progeny.
FAQs
Q1: What is the life expectancy of someone with primary ciliary dyskinesia?
Ans: According to some reports, PCD is linked to chronic respiratory diseases, which may shorten lifespan. Although this reduction is not as severe as that seen in other similar disorders like cystic fibrosis, some individuals suffering from PCD have lived into their 70s or 80s.
Q2: Is primary ciliary dyskinesia dominant or recessive?
Ans: In PCD, the inheritance pattern is of the autosomal recessive type. Only when a person receives the identical abnormal gene for the same trait from both parents do recessive genetic disorders develop.
Q3: What’s the difference between primary ciliary dyskinesia and cystic fibrosis?
Ans: The roots of the two diseases are different: On one hand, PCD arises from the malfunctioning of the cilia, which usually participate in sweeping mucus out of the respiratory tract. Contrarily, people with cystic fibrosis experience difficulties moving water and salt across cell membranes, which results in the production of abnormally sticky mucus.
Q4: How do you test for primary ciliary dyskinesia?
Ans: PCD is diagnosed through examination of tissue of the lung or sinus obtained from a biopsy or through genetic testing. Specific structural defects that are present in these tissues can be detected under an electron microscope.
Q5: What is the treatment of primary ciliary dyskinesia?
Ans: There is no absolute cure for PCD. But treatment slows down disease progression. Therapists may prescribe antibiotics along with bronchodilators or anti-inflammatory medicines. These medicines help in treating lung infections, opening up the airways, and reducing swelling.